|
Conversations with Neil’s Brain The Neural Nature of Thought & Language Copyright 1994 by William H. Calvin and George A. Ojemann. You may download this for personal reading but may not redistribute or archive without permission (exception: teachers should feel free to print out a chapter and photocopy it for students). William H. Calvin, Ph.D., is a neurophysiologist on the faculty of the Department of Psychiatry and Behavioral Sciences, University of Washington. George A. Ojemann, M.D., is a neurosurgeon and neurophysiologist on the faculty of the Department of Neurological Surgery, University of Washington. |
|
The Problems with Paying Attention WE WERE SITTING ON THE PARK BENCH behind the medical center, our attention riveted on a particularly handsome sailboat that was idling impatiently in midchannel, waiting for the drawbridge to go up. Attention is the gateway for memory — which is why I still remember that sailboat with its sails unfilled. If you don’t pay attention to something at the time it happens, you are unlikely to be able to recall it tomorrow. That isn’t to say that you can’t “play back” a strange noise that awakens you in the middle of the night. Or recall a conversation that you accidentally overheard while talking to someone else — provided that you start mulling it over within the next few minutes. But memory works best for what you had your attention focused on at the time, and gradually recall becomes impossible for anything else. “So what kinds of memories do you suppose I’ll recall when George stimulates my temporal lobe?” Neil asked. He was, I noticed, jumping the gun a little, as I knew that George wanted more tests before going ahead with a decision to operate. Probably nothing will flash into your mind, I said. Wilder Penfield’s “experiential responses,” which everyone seems to have heard about, are actually infrequent. Experiences evoked by electrical stimulation happen to less than one patient in a dozen in the published studies, and George sees even fewer. They’re nearly always from temporal lobe. Sometimes they’re impressively detailed, but usually they’re just voices heard offstage. George once had a patient who heard Led Zeppelin music each time a particular temporal lobe site was stimulated. Sometimes it was the same song, sometimes a different one from the same album. “So that’s the impact of decades of Top 40 Radio. They no longer have to be broadcast — by now it’s all imprinted!” Penfield got many reports of lullabies and classical music, too. Sometimes the recall was a particular piece of music, sometimes a specific scene from the patient’s past — such as Penfield’s patient who recalled her mother talking to her aunt on the telephone about a visit. Usually it wasn’t a complex “multimedia” hallucination but just some unidentifiable experience. Penfield, especially after he retired as director of the Montreal Neurological Institute in 1963, emphasized his belief that memory is like a tape recorder, capturing and storing all the detail. That’s easily the most widespread popular belief these days as well. Back in 1980, a survey showed that even most psychologists believed in a videotape analogy. “Videotape is probably the only technological analogy available to most people.” But modern memory research tends to dispute the videotape metaphor, emphasizing that attention is needed at the time, and that what does get stored is surprisingly malleable, easily distorted by later events. In particular, things tend to get “out of order,” mistakes being made about what event followed another, in a manner that videotape doesn’t do. And modern neurosurgeons tend to think that those stimulation-evoked “experiences” are actually little seizures that evoke hallucinations — that they are more like the fragments of our nighttime dreams than like a fully formed sensory experience being replayed. “So what happened? Did these people have a seizure at the same time as this experience, that burned in the details?” That’s possible. Patients who have experiential responses from temporal lobe stimulation are also particularly likely to have them as part of their seizures as well. But this could be just an accidental association. Certainly it’s not just a matter of the stimulated site. George likes to go on — using in his mock-ominous tone of voice again — about his patient who heard Led Zeppelin music, saying the patient’s “Led Zeppelin area” was naturally removed since George dislikes such music. Some years later, George then reveals, he was talking to the patient about that experience. George asked the patient if he remembered the moment in the operating room when he heard that music. Yes, indeed. Then George asked if his musical interests had changed after the operation. “Oh yes,” came the patient’s reply. “I’m into deep rock now!” Removing that whole section of temporal lobe (the Led Zeppelin area was, of course, part of the epileptic focus and scheduled for removal anyway) didn’t eliminate the patient’s abilities to recall the music or the experience afterward. So it was hardly the sole site of memory storage. One of the reasons people now believe that these “recalls” are just seizure-associated hallucinations is that all of the more complex ones are associated with minor seizure activity — what we call afterdischarges — both locally and in the deeper structures of the temporal lobe. And the more you turn up the strength of the stimulating current, the more likely you are to evoke these reports — and to see afterdischarges spreading more widely. “Does it cause a full-blown seizure?” Neil asked. If the current is strong enough and lasts long enough, even normal cortex can be pushed into a seizure. That’s one way psychiatrists produce seizures during electroconvulsive shock therapy for severe depression. In the O.R., we always keep the strength below the threshold at which afterdischarges start to occur locally, and well below the threshold for its spreading outside the local area. |
|
SEIZURES COME IN ALL SIZES. There are little seizures and medium-sized seizures. And
then there are big seizures. “I hate the big ones,” Neil said. “I’m unconscious, just like in the little ones. So it’s not that. But everybody says I put on a show with the big ones, stiffening up and then jerking all over. It’s embarrassing as hell. Sometimes I lose my urine and bite my tongue. Then I always feel groggy and sore all day.” Every part of the cerebral cortex is capable of going into a seizure if provoked hard enough. What provokes it is usually a seizure in a neighboring area, so the seizure may spread like a burning fuse, involving one area after another. “But my big seizures come all at once. Both arms and legs, and on both sides of my body, all at the same time.” That’s what’s called generalization of the seizure, I told him. An EEG then will show epileptic activity on both sides appearing all at once, at the same time as the patient suddenly stiffens. It’s as though some mechanism had spread a small seizure throughout the whole brain instantly, the way an aerial bomb blast can start many widespread fires at the same time. The major effect of the anticonvulsant drugs is to prevent that kind of spread. Sometimes the generalized seizure seems to be the only kind of seizure a patient has, which deprives the neurologist of the best clues. Such a seizure could have started almost anywhere in the brain. It’s only the beginnings of a seizure, before generalization, that can tell you where the trouble is. If the patient has little seizures in between the medium and big ones, the neurologist has much more information for locating things. “Mine start when I go blank. I’m sort of `out of it’ despite still sitting there at the dinner table. Sometimes I may start tapping a spoon on my plate. Or chewing and swallowing, even though dinner hasn’t been served yet.” Now, to a neurologist, that immediately waves a red flag. Automatisms can originate from almost anywhere in the temporal lobe, but seldom from any other part of the brain. What else happens to you, especially before those automatic movements? “Well, mostly I don’t remember very well. But often there’s an awful smell. I don’t really know how to describe it — it’s not like anything real. Maybe a bit like burning rubber. And that’s the last thing I remember.” Those kinds of hallucinations are known as the “aura” of a seizure. They’re actually little seizures and, at least when we can find their source, we tend to call them focal seizures. That particular kind, associated with a brief unpleasant smell, often can’t be seen on the EEG recordings from the scalp. With smells like that, there is usually a small seizure occurring in the uncus, the inner part of the temporal lobe that bulges out, almost touching the brain stem. “That’s what my doctor said.” When they involve automatic actions like fumbling with a spoon and chewing without food, with no memory for these actions, we’re more likely to call them complex partial seizures. Patients are likely to take about half an hour to fully recover from one of these, although they are unresponsive for only a few minutes. That kind of seizure is more likely to show up on a scalp EEG, in which case they’re often localized to the temporal lobe. Patients report a variety of feelings and experiences with temporal lobe seizures. Some experience déjà vu, that feeling of unusual familiarity, as though they had been here before. Or illusions — for example, distortions of size or shape in which individuals appear as giants or little people. Some suffer hallucinations, auditory or visual — even smells. “My neurologist told me about a patient of hers who saw a bucolic farm scene before each seizure. The patient even drew the scene for her. It sounds like `visions’ from the Bible or some such thing.” Paul’s vision on the road to Damascus, sure. Maybe he had temporal lobe epilepsy. The voices that told Joan of Arc to save France may well have been auditory hallucinations with temporal lobe seizures. They say that when Joan was burned at the stake, her heart wouldn’t burn. One thing that could cause that is calcification of the covering of the heart — calcific pericarditis — which is a consequence of tuberculosis. Brain tuberculomas - little tumors of tubercular tissue - are common in widespread tuberculosis, and seizures are a common symptom of those tumors. So it wouldn’t be surprising if she suffered from little seizures in the temporal lobe. “Temporal lobe epileptics are such interesting company — Dostoyevsky, van Gogh. I’ve heard it said that Jonathan Swift and Lewis Carroll probably had it too, because of all the little people they wrote about in Gulliver’s Travels and Alice in Wonderland.” Yes, seeing giants and little people can be symptoms of temporal lobe seizures. If they never progress to bigger seizures, they may never get diagnosed as epilepsy. “So what’s the difference between the little seizures and the big ones?” The big seizures — grand mal or just generalized seizures — start out the same way as the littlest. But they recruit more followers and so progress further through the brain. “I can never tell if one of mine is going to be big or little.” The big ones don’t stop with fumbling movements. All of the sudden, a patient will stiffen all over. When I was out shopping last year, I saw a guy stop in the middle of the sidewalk. He looked confused and swallowed repeatedly. After maybe ten seconds, he looked like a frozen statue, his right forefinger pointing toward heaven. His head was drawn back, so it looked as if he were gazing toward heaven as well. “Sounds like a lot of religious paintings I’ve seen from the Middle Ages. The saints, frozen just like that.” Hippocrates, in the fifth century b.c., called epilepsy “the sacred disease.” But this man on the sidewalk: after a few seconds of this frozen posture, both of his arms began to jerk, as if he were gesturing to the gods, jabbing with that forefinger. And his legs jerked too. He would have toppled over if two companions hadn’t grabbed him. They laid him down on his side and folded a coat under his head, which is exactly the right thing to do. They looked so competent that I just sat in my car and watched as they reassured the pedestrians. The jerking stopped in a few minutes, but it was fifteen minutes before he was sitting up. He looked hungover but five minutes after that, he was able to walk away looking fairly normal. “After I have one of those, I just get my secretary to cancel my appointments and drive me home. Complete loss of the day.” There are other kinds of generalized seizures that are basically inhibitory, like briefly turning off a switch. Those patients tend to look awake but briefly out of contact. This seizure type is more common in kids. These seizures are sometimes called absence, pronounced as in French — the name probably derives from the phrase, absence d’esprit, or “absence of mind.” In the old terminology, the French and everyone else called them petit mal — the “little sickness.” “So what spreads the focal seizures around, to make a big one?” They co-opt the selective attention circuitry. Some neurons seem to have connections to everywhere, such as those neural circuits that help keep you awake and alert. Remember when we were discussing coma, particularly those serotonin and norepi connections from the brain stem that spread diffusely through the cortex? The ones I likened to underground lawn sprinklers, spreading liquid fertilizer to grow thoughts? “So the seizure spreads into that system and then gets broadcast everywhere?” Well, that was Penfield’s notion, although it may require some neural connections that aren’t very obvious. Since then, another possibility has appeared, that there is wrong-way impulse traffic in that attention system. Just imagine that plumbing system working backward, as if someone were forcing water from a hose down one of the sprinkler heads, and it came back up through all the others. Neurons are normally one-way streets, but occasionally they can be forced into working backward. |
|
SELECTIVE ATTENTION seems like a spotlight, highlighting some aspects of the sensory
environment while keeping others in the background. We appear to use the same system to focus inward, the way you’d try to remember the name of someone you saw years ago, while trying to ignore the distractions of the sights and sounds of the cafeteria. This is the circuit that selects which sensations we will emphasize, out of the many we are exposed to. What we store in memory, what we retain as our conscious experience. Which we will try to recall from memory. So selective attention is perhaps the closest we will come to finding one system in the brain that determines the current content of our conscious experience. “Now we’re getting somewhere. So that’s the real me? Selective attention is like a television producer in the control room, deciding which camera’s view should go out over the air?” Sometimes the spotlight can’t be moved very well, as in those right-brain patients who neglected things to their left. That’s an example of a posterior parietal lobe area that is involved in focusing selective attention, and the plumbing of that norepi system seems to favor such areas. Drugs that reduce the effectiveness of norepi interfere with the ability to focus your attention, as in paying attention to what the teacher is writing on the board.  [FIGURE 28 Selective attention specialties] Some blood flow studies of the brain have been done during vigilance tasks, such as watching for the traffic light to finally change to green. These are very much right-brain tasks, involving both that posterior parietal area and a region of frontal lobe. And you see exactly the same two areas light up even if it isn’t a visual task, such as waiting for a tap on the big toe. Various parts of the frontal lobe and brain stem are used in orienting toward a stimulus, as when a cat hears a noise, then turns her eyes, points her ears, and finally rotates her whole head around toward the source of the sound. But that seems to be different from staying alert for a particular type of stimulus — what we’d use to listen for a baby crying upstairs in the midst of traffic noises from outside. The frontal lobe is particularly involved in representing things during their absence, and you seem to use some regions of the midline regions of the frontal lobe, the cingulate gyrus just in front of the corpus callosum, to stay alert for a class of words — such as when you are looking for Italian surnames while scanning a telephone book. Both anterior and posterior attention systems have many subcortical partners in doing their job, especially in the thalamus. The brain stem mechanisms for arousal from sleep are a fairly general system, but the high-end version of the system in the thalamus is somewhat more specific. 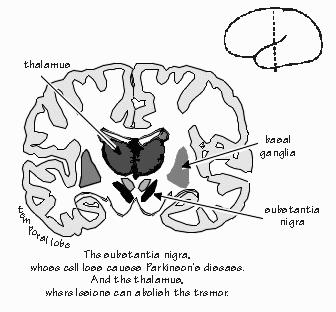 [FIGURE 29 The substantia nigra, thalamus, and basal ganglia] |
|
WHILE THE THALAMUS isn’t really the center of things — the thalamus and
frontal cortex are a closely linked system — some of the best examples of how selective
attention works come from operations on the thalamus, which are done for the treatment of
Parkinson’s disease. A little microtremor is normal. But a year or two after a patient thinks he just has the coffee jitters, he starts having more than the usual problems with writing checks. Or swinging an arm. Or cutting steak with a knife. The stiffness finally shows up in overall posture or in a shuffling gait. The voice often fades. So it’s the stiffness and the tremor that finally prompt a visit to a neurologist. And the neurologist will try to explain that some neurons that make dopamine — one of those neurotransmitters with a broad distribution like serotonin and norepi — aren’t doing a very good job of it anymore, because many of them died decades earlier. There is a drug, L-dopa, that helps the remaining neurons of the substantia nigra to manufacture more dopamine, and that often helps. But some of the patients will still have a tremor, even though their stiffness is satisfactorily controlled by the drug. It’s those patients who may benefit from an operation on the thalamus. “I thought that the trouble was in the substantia nigra,” Neil said. That’s the pigmented region of the brain below the thalamus, from which many neurons are missing. The thalamus is probably normal. However, most brain systems are really two systems, one pushing while the other pulls. What’s so important is the balance between them. Killing a small portion of thalamus seems to roughly compensate for the loss of those neurons in substantia nigra, reestablishing a balance in the system that regulates tremor. “So how do you get to the thalamus if it’s so deep inside the brain?” Through a little hole in the skull, positioned over an area without major blood vessels. It’s all done with local anesthesia. The neurosurgeon just sinks a needlelike probe down about three inches into the thalamus and coagulates a little of the thalamus around the tip of the probe. The patient’s tremor usually stops immediately. The trick is in knowing how to aim the needle and how to be sure where the tip is. “No kidding. `These are professional surgeons, kids — don’t try this at home.’ So how do they know where the tip is located — using X-rays?”  [FIGURE 30 Testing Neil’s memory with a three-slide sequence] Right, but since brains vary in function as well as anatomy, neurosurgeons tend to stimulate from the tip of the probe while asking the patient to perform some relevant task. One of the tasks George uses when he does a thalamotomy for parkinsonism is to have the patient watch a projection screen while slides are shown. First, there is a slide showing some common animal or object, such as an elephant. So the patient says, “This is an elephant.” Then it gets more interesting. A second slide pops up, and all it shows is a number. The patient, being well-rehearsed beforehand, starts counting backward from this number. Then about six seconds later, a third slide pops up, that says simply “Recall.” The patient is supposed to recall the name of the object on the first slide: “Elephant.” But you can make this task harder, so that the patient will make errors half of the time. Just have the patient count backward by threes. Then the patient has a harder time hanging on to the elephant name over the distracting task. If George adjusts the difficulty of the task so that the patient normally makes errors in recall about half the time, he sees a very interesting effect of stimulating the thalamus while the elephant or whatever is on the screen: not only is naming more accurate, but there aren’t as many recall errors later. Stimulation makes memory better! “What happens if George stimulates during the other two slides?” The patient will be able to count backward during thalamic stimulation, but during the third slide — with the current turned off — he’ll remember only about half the names. Same as without stimulation. Stimulation during the third slide results in many more errors. So it looks as if the thalamic stimulation made the patient pay attention to what he was seeing at the time. Thus, stimulation during the first slide improved his recall during the third. And stimulation during the third slide forced his attention toward the screen rather than allowing him to focus inward, to retrieve the prior name. The selective-attention circuit was acting like a gate, allowing information into or out of recent memory, but not both at the same time: you either daydream or you pay attention to me, but not both. Paying attention conflicts with recalling things from short-term memory. “Short-term memory? There’s another kind?” Neil asked with a smile. “I’ve begun to wonder why names keep slipping away.” Immediate “working” memory, short-term post-distractional memory, and long-term consolidated memory seem to involve different brain mechanisms. But I can’t explain them — and certainly not the “memory problems” that people complain about — until we discuss those synapses and electrical signals inside neurons. All of this, so far, is for patients having an operation on their left thalamus. But the right thalamus sometimes gets operated on too, and the results in those patients are quite different. Object form and shape, rather than words, are selectively attended to and remembered. George often uses slides showing complex shapes. After the distracting task of counting backward, the patient is asked to pick which of three shapes was the one he saw earlier. “So what happens?” Same thing as with left thalamic stimulation: recall is improved. But what’s really interesting is if there is a conflict between right and left thalamus, between names and lines. Stimulate the right thalamus when the patient is naming objects, and there is no special effect. Stimulate the left thalamus during object naming, and you get improvement in recall later. But if you show complex shapes while the left thalamus is being stimulated, there will be many more errors — as if the shapes were being ignored while the left thalamus was stimulated. The left selective-attention system directed at retaining verbal information dominated the choice of what was to be selectively retained from the environment. As George says, it shows true dominance of the left brain over the right brain — not in general, but for this particular aspect of selective attention. |
|
OUR PERCEPTION OF THE WORLD depends first on what our sensors detect — for
example, we can’t see the infra-red of heat, or the ultraviolet that gives us sunburn. But
second, it depends on what our selective-attention circuits select from all the sensations. What
gets through that set of filters is what we might retain in memory. That makes selective attention circuits very important for learning. They allow you to acquire new information more reliably. When selective attention is not directing you toward the external world, you can browse through your memories, either in search of someone’s name or that more free-form retrieval we call fantasy or daydreaming. Defective function of these circuits seems to be the basis for attention deficit syndrome and minimal learning disorders, situations in which a child has difficulty sustaining attention. These might well involve those selective-attention circuits passing through the left thalamus that focus attention on verbal information such as object names. More severe malfunctions in these circuits are probably a part of autism, in which there is an overall limitation in attending to the external environment, especially in attending to the presence of other people and perhaps to verbal information. This limitation is coupled with severe distractibility and an intense focusing of attention on a limited selection of environmental features. The brain circuits that are defective in autistic children are not well established. While many of their problems with imagination and social inappropriateness are reminiscent of frontal lobe patients, subtle disorganization of neural circuitry has been found in both thalamus and the language cortex. Their behavioral pattern suggests that very poor function of thalamic selective-attention circuits is likely to be present, as though the autistic child is largely oriented only to what has been previously acquired, and limited in the ability to acquire new material from the environment. They’re stuck. Although many autistic children are also mentally retarded, not all are. But even the brighter ones have trouble with make-believe, such as pretending to feed a doll with an empty spoon, and may not understand that other persons may have different viewpoints and beliefs. And even the more able autistic individuals may have a hard time making a mental model of another person’s state of mind. They cannot understand deception. Being so literal, they don’t appreciate humor or irony, can’t read between the lines. They lack a “theory of mind” with which to understand others. Sometimes autism is the result of brain damage in early life. Sometimes there seems to be a genetic component. If one of identical twins is autistic, the probability is very high that the other one will be; for fraternal twins, who do not have identical genes, that probability is very low. “I wish I’d had one of those thalamic electrodes in place when I had to learn Spanish. I could have turned it on each time I had to learn a new word and retained it better for the exam.” Yes, but if you’d accidentally turned on the stimulator during the exam, you’d have remained focused on the questions and unable to retrieve the answers from memory. We joke a lot about medical students wanting a thalamic stimulator while learning gross anatomy. But someday we might be able to use one with certain kinds of autistic kids to help them out of their withdrawal. “What gets to me,” Neil said as we prepared to leave, “is that this isn’t science fiction. Everything you come up with in real science seems to open up a whole new set of possibilities.” And mostly in applications that we’d never have guessed. |
 Conversations with Neil's Brain:
Conversations with Neil's Brain: The Neural Nature of Thought and Language (Addison-Wesley, 1994), co-authored with my neurosurgeon colleague, George Ojemann. It's a tour of the human cerebral cortex, conducted from the operating room, and has been on the New Scientist bestseller list of science books. It is suitable for biology and cognitive neuroscience supplementary reading lists. ISBN 0-201-48337-8. | AVAILABILITY widespread (softcover, US$12).
|